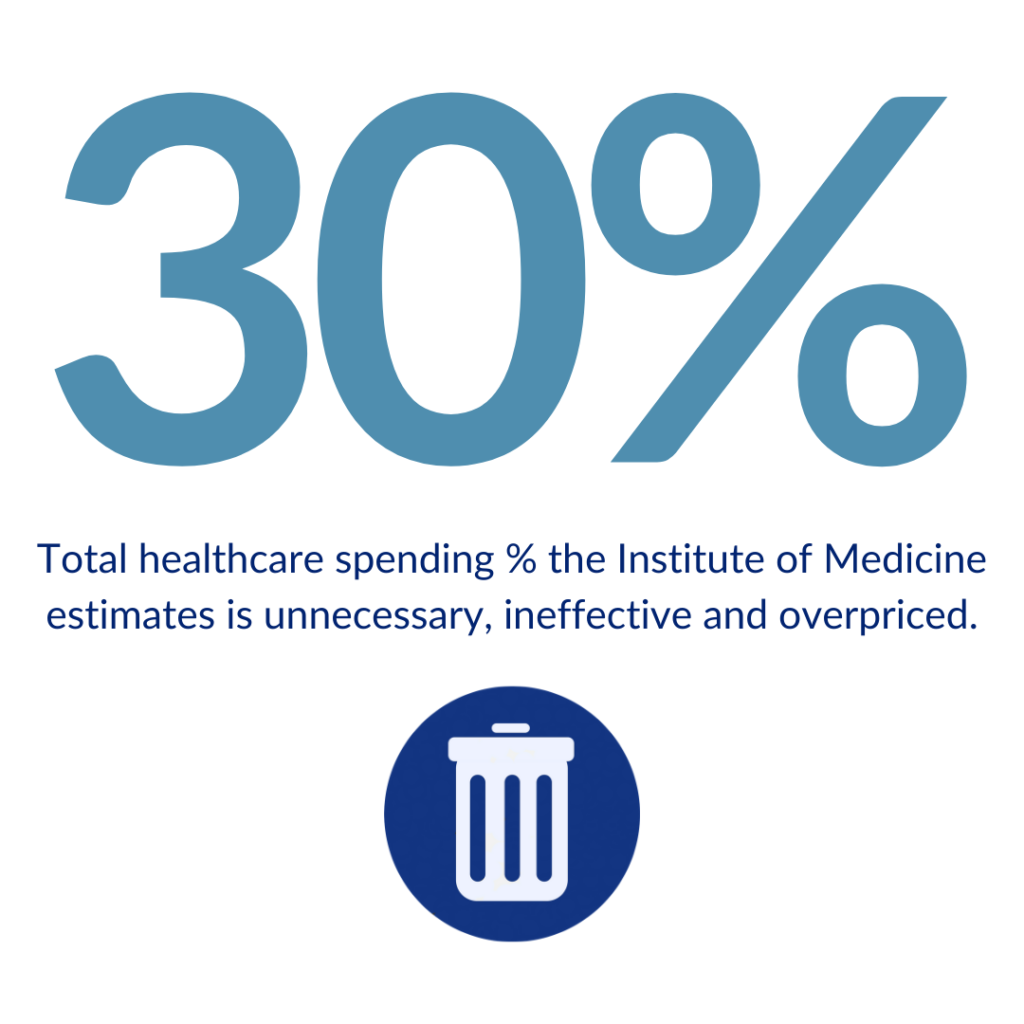
Billions are wasted annually in self-insured employee health care plans.
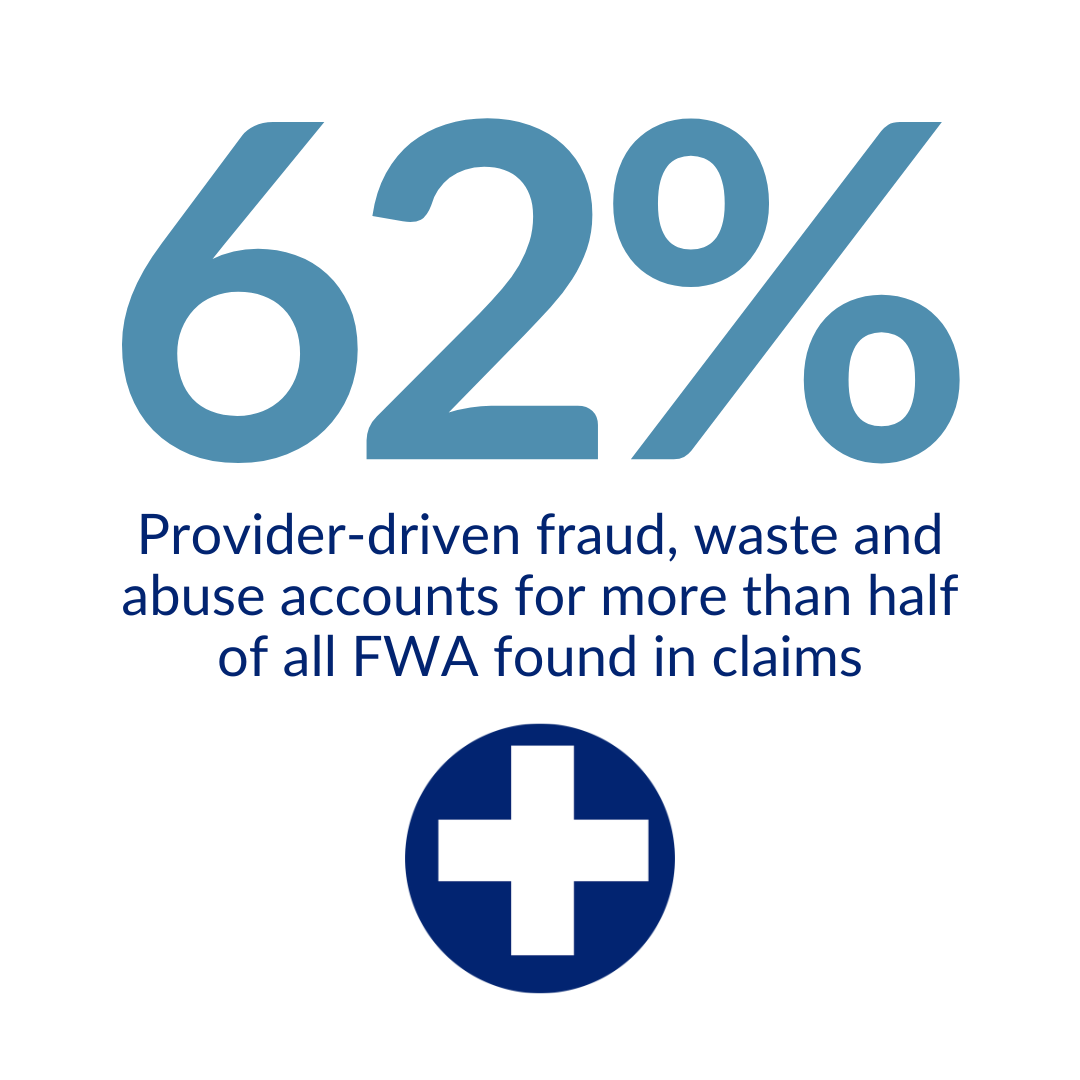
If you are an employer with a self-funded health care plan, you are losing money to fraud, waste and abuse. This waste, hidden within your health care claims, contributes to the ever rising cost of your health care benefits budget.
Employers and third-party administrators often don't know issues exists within their claims.
Do you know if your claims contain:
- Abusive Billing
- Services Not Rendered
- Pricing Failures
- Non-covered Services
- Duplication of Services
- Billing Errors
- Payment Errors
- Drug-seeking Behavior
- Overtreatment
Having a regularly scheduled and monitor claims review process in place has proven to:
- Reduce unnecessary health care claim payments
- Prevent waste and fraud from happening in the first place
- Help employers manage their spend more efficiently
The well-documented issue of rising health care costs:
- We all pay the price with increased premiums and health care costs. A Washington Health Alliance analysis recommends a critical eye toward eradicating overuse of low-cost services. Read more about the report here. U.S. spends far more on healthcare than other developed countries—and researchers say prices are still to blame. Read piece on fiercehealthcare.com
- SHRM says employers will spend nearly $15,000 per employee on health benefits in 2019. Read their forecast.
"SmartLight is a great partner. They are finding some very real issues and creating significant savings."
-Nathan Gregory, SPHR, SHRM-SCP, City of Fort Worth Assistant Director of Human Resources



